STATE-OF-THE-ART REVIEW • Ultrasound Imaging of the Abdominal Aorta: A Comprehensive Review
Source: Ultrasound Imaging of the Abdominal Aorta: A Comprehensive Review
INTRODUCTION
Ultrasound imaging as an imaging modality for the abdominal aorta (AA) is highly valuable due to its high diagnostic yield coupled with advantages that include a noninvasive approach, cost-effectiveness, capability for point-of-care imaging, absence of procedure-related complications, lack of ionizing radiation and iodinated contrast use, and relatively short procedural duration.
Ultrasound allows the identification and assessment of structural abnormalities of the AA, including aneurysms, atherosclerosis, thrombosis, dissection, and arteritis, among other pathologies.
Ultrasound as done in vascular and radiology laboratories typically involves imaging of the entire AA, is performed in a fasting state by personnel trained in general and/or vascular ultrasound, uses a curvilinear transducer, and aims primarily at identifying structural abnormalities of the AA. Conversely, imaging performed in echocardiography laboratories as part of a transthoracic examination is typically limited to the proximal segment of the AA as visualized from the subcostal window, is performed in a non-fasting state by personnel trained in cardiac ultrasound and using a phased-array transducer, with the main purpose of obtaining anatomic and hemodynamic information pertaining to disorders that involve the heart and vasculature.
The aim of this review is to demonstrate the usefulness of ultrasound imaging for the detection and evaluation of disorders that involve the AA, detail the abnormalities that are detected or further assessed, and outline its value for echocardiographers, sonographers, and radiologists.
ULTRASOUND IMAGING OF THE AA
Image Orientation
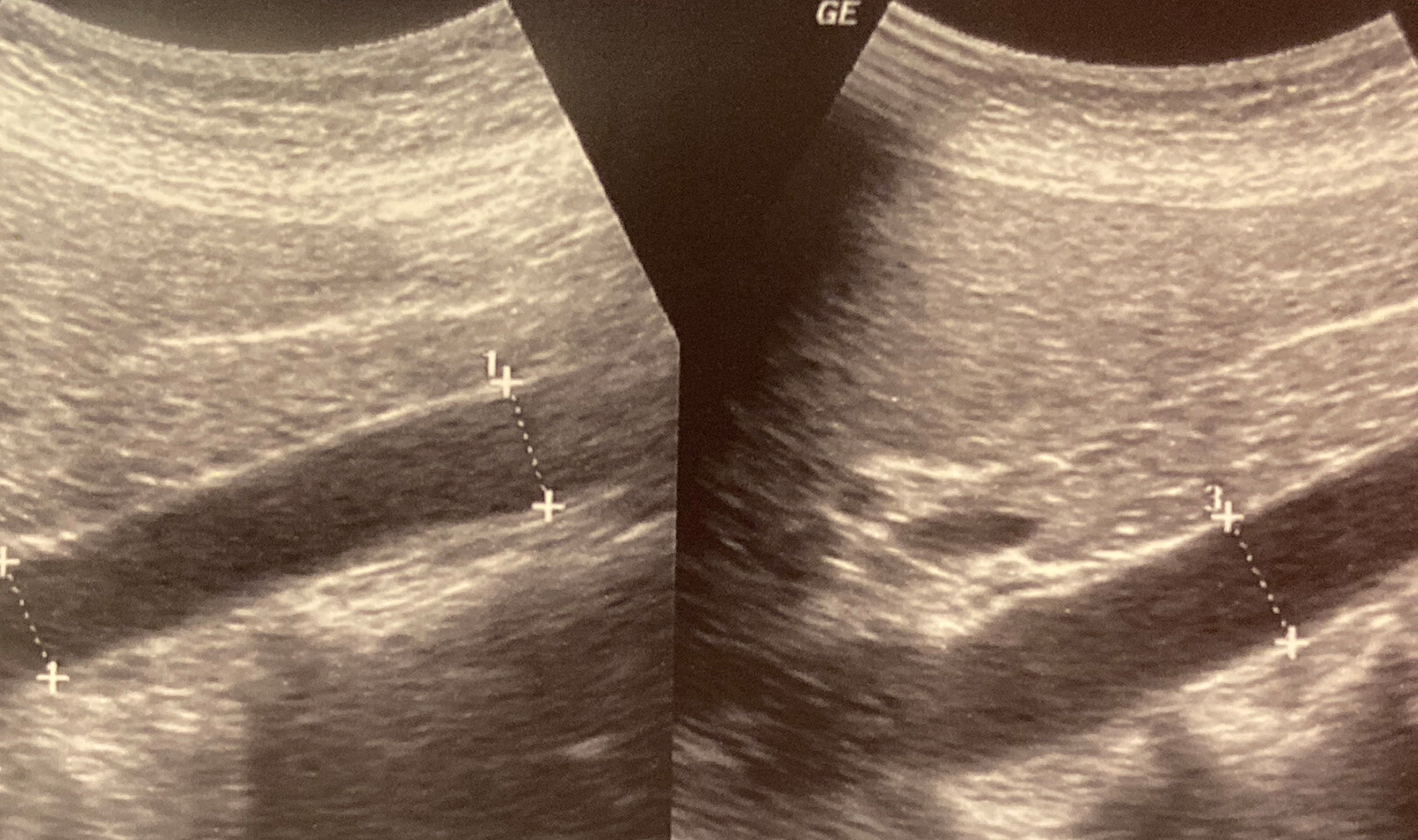
In the supine position, scanning from the subcostal window to the level of the umbilicus allows visualization of the AA in its entirety. The longitudinal view is obtained in the sagittal plane with the transducer positioned along the long axis of the AA and its notch pointing toward the patient’s head. This view allows measurement of the anteroposterior (AP) diameter (front to back) of the AA and the length (cranial-to-caudal) of any structural abnormality, but it does not allow width (side-to-side) measurement.
Ultrasound Transducers
Abdominal ultrasound is performed with 1.5- to 6.5-MHz curved-array probes that have a large footprint, wide beam point, and convex beam shape, thus allowing a wide field of view and optimal imaging of the AA.
Measurement of the Dimensions of the AA by Ultrasound
Accurate measurement of the maximal diameter of the AA is essential, particularly in the setting of an AAA to establish an indication for intervention or future monitoring. Discrepancies and/or inaccuracies in diameter measurement may result in overtreatment or undertreatment of patients.
There is no consensus regarding the best method for measuring the AP and transverse diameters of the AA by ultrasound. Three methods are currently in use, including outer wall to outer wall (OTO), inner wall to inner wall (ITI), and leading edge to leading edge (LELE).
Ultrasound- versus CT-Derived Dimensions of the AA
While CT is the gold-standard modality for quantification of AA dimensions, screening for AAA, follow-up evaluation, and diameter cutoffs for intervention are based mostly on ultrasound-derived data. An important difference between CT and ultrasound is the use of the largest aortic diameter in any plane by CT versus the use of only the AP and transverse diameters by ultrasound, with ultrasound diameters measured perpendicular to the aortic lumen.
Imaging of the AA by Transesophageal Echocardiography
Transesophageal echocardiography (TEE) allows imaging of the suprarenal portion of the AA. The celiac artery and superior mesenteric artery (SMA) can often be imaged from the transgastric window.
Normal Flow Pattern in the Proximal AA
Pulse wave Doppler interrogation of the proximal AA typically demonstrates a triphasic pattern including a prominent anterograde systolic wave with rapid acceleration and deceleration time, a low-velocity early diastolic reversal (DR), and low-velocity anterograde flow that may persist throughout diastole.
Normal Flow Pattern in the Distal AA
Doppler interrogation of the distal AA beyond the IMA typically demonstrates a biphasic flow pattern, including a systolic anterograde wave and an early DR. The systolic wave has a lower velocity, whereas the DR often has a higher velocity and longer duration than in the proximal AA.
The paper continues to review abnormalities on 2D and 3D imaging of the abdominal aorta such as abdominal aortic aneurysms, ultrasound imaging following endovascular aneurysm repair, pseudoaneurysms, atherosclerosis, penetrating aortic ulcer, thrombi, aortic dissection, and arteritis.
In addition, it describes the spectral Doppler interrogation abnormalities of the abdominal aorta. This includes disorders of the aortic valve such as aortic regurgitation, coarctation of the aorta, takayasu arteritis, and others.
 English
English
 Español
Español