ORIGINAL RESEARCH • Diagnostic Utility of Point of Care Ultrasound in Identifying Cervical Spine Injury in Emergency Settings
Source: AJUM November 2021:24(4):208-216
INTRODUCTION
Cervical spine injury (C-spine injury) is the most common debilitating injury among spinal cord injuries. Evaluation of patients with a suspected C-spine injury is done with variable accuracy using clinical decision-making tools such as NEXUS criteria and Canadian C-spine rule. A considerable amount of variation exists with radiological evaluation. X-ray was used for decades and consisted of a 3-view cervical spine series. However, this conventional series of X-rays reported up to 35% of missed C-spine injuries. CT scan has emerged as a good screening tool in C-spine injury due to its high negative predictive value. However, in a hemodynamically unstable trauma patient, many clinical guidelines do not recommend CT scan, which results in delayed clearance of C-spine in these unstable patients.
Since the application of a rigid cervical collar for a short period can result in a change of optic nerve sheath diameter in healthy volunteers, and prolonged immobilization of C-spine is associated with an increased risk of pressure sores and raised intracranial pressure (ICP), the ideal C-spine clearance protocols must balance the risk of missed injury against the potential for increased morbidity from prolonged spinal immobilization.
Therefore, the goal of this study was to evaluate the use of POCUS for identifying cervical spine injuries.
METHODOLOGY
This was a single-center, cross-sectional study conducted at a level 1 trauma center over 18 months.
The primary objective was determining the ability of POCUS to detect c-spine injuries in proven cases of c-spine injury.
The secondary objective was to study the normal anatomy of the c-spine in patients without c-spine injury and user-friendliness of probes (curvilinear vs. linear) in terms of image acquisition, optimization, and interpretation.
The study was conducted in two phases. In phase one, two emergency physicians (EPs) were trained over 3 months in the POCUS algorithm to identify c-spine injury under the supervision of an emergency medicine consultant who is an expert in emergency ultrasound to standardize the technique.
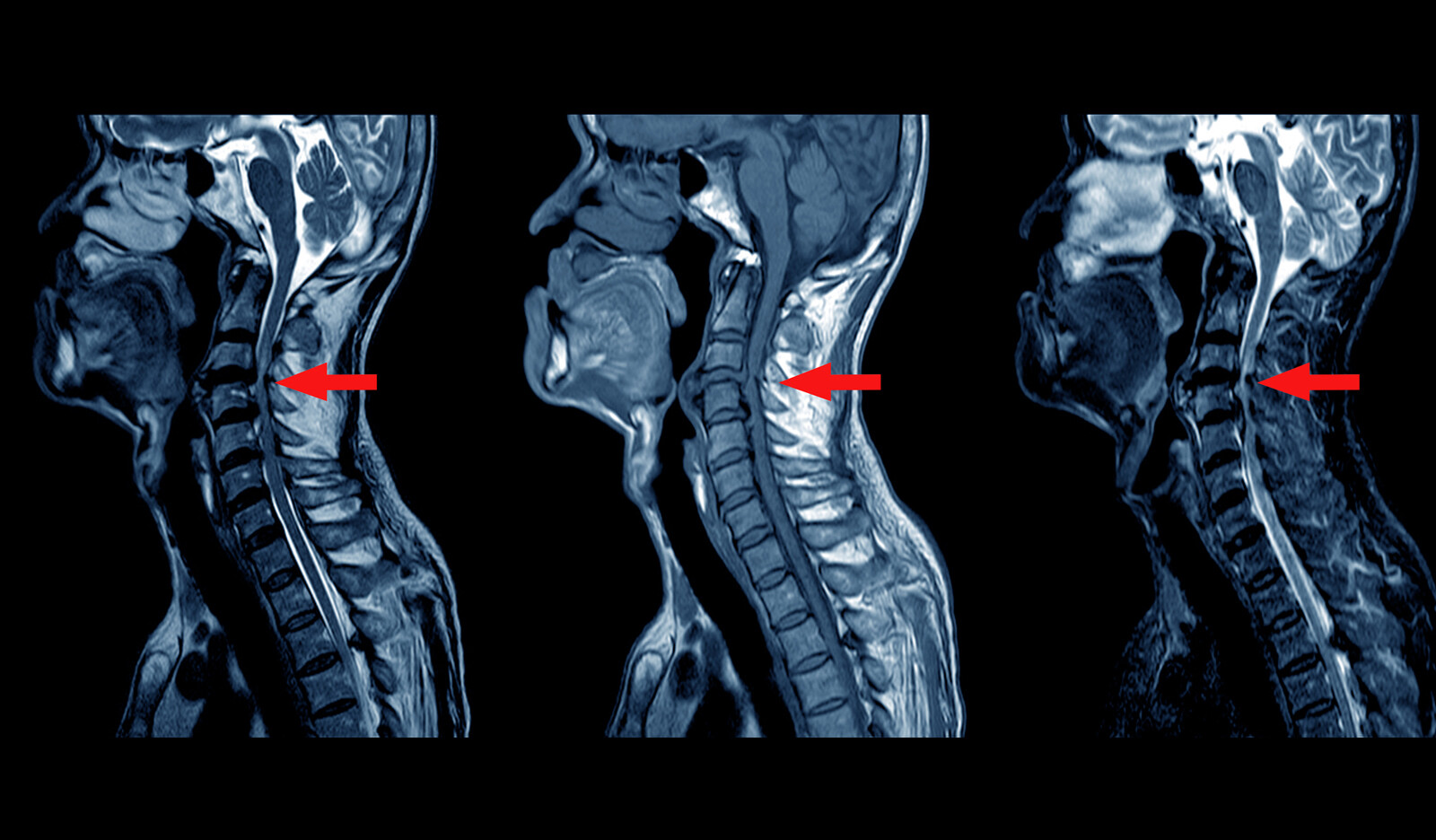
In the second phase, all patients over the age of 18 months, who had a suspicion of cervical injury based on NEXUS criteria, were screened and a cervical CT was performed. The patients with cervical spine injury were triaged as red and observed in the Emergency department (ED) for admission. The EPs performing the ultrasound were not part of the trauma resuscitation team. The ultrasound images were recorded independently by the recruitment team. Patients with a focal neurological deficit but a normal CT scan underwent magnetic resonance imaging (MRI).
CT findings were interpreted separately by the radiologist. The EPs performing the POCUS were blinded to the finding of the CT/ MRI. Those with positive CT findings were included in the study. The patients with no neurological deficit and normal CT scan were excluded. After every 5 scans, the images were verified by the consultant for image acquisition, optimization, and interpretation.
RESULTS
Cervical ultrasound was done in 84 patients with CT/MRI-confirmed C-spine injury. The average age in C-spine injury (group II) was 37.2 Æ 14 years with 72 males (85.7%) and 12 females (14.3%). The commonest vertebral fracture (including body and posterior elements) observed by CT scan was C6 (C6 = 24; C5 = 23; C7 = 19; C4 = 10, C2 = 8, C3 = 3; C1 = 1).
Based on CT scan, 51% (43/84) had injury involving more than one vertebra. There were nine (11%) cases of upper cervical spine injury (C1 and C2) and 63(76%) cases of lower cervical spine injuries.
Normal anatomy on POCUS
Vertebral bodies were seen as blocks with a concave anterior surface in the anterior longitudinal axial scan. Maximum visibility was from C3 to C7-T1 junction. POCUS could also visualize cervical lordosis, intervertebral disc spaces and anterior longitudinal ligament (ALL).
The quality of images was better with the linear probe when compared to the curvilinear probe. However, only two vertebrae were seen in a single window and the alignment was not visualized. The optimal image was obtained by adjusting the depth of the linear probe to 4 cm and directing the plane through the carotid artery or internal jugular vein.
Upper cervical vertebra (C1 & C2), transverse processes and elements of the posterior column (articular process and facet joints, pedicle, lamina, and spinous process) were not visible by the anterior approach.
Injury patterns identified by POCUS
POCUS identified 22/26 (84%) cases of listhesis. Out of 26 cases of listhesis, one had hangman’s fracture with C2-C3 listhesis which was not visible on POCUS. POCUS identified six out of seven cases of C4-C5 listhesis and eight out of nine cases with C5-C6 listhesis. POCUS detected all 8 cases of C6-C7 listhesis and missed one case of C7-T1 listhesis.
There were 6 cases of false-positive listhesis. Three had vertebral body fractures in CT scan. Three had osteophytes and diffuse idiopathic skeletal hyperosteosis which was mimicking listhesis.
The overall sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of POCUS vs CT scan for vertebral body listhesis are 84.5%, 89.7%, 78.6%, and 92.9% respectively.
Vertebral body fractures
Out of 84 patients, 22 had vertebral body fractures diagnosed on CT. Of these, 9 cases were identified by POCUS.
Most involved vertebra in CT scan was C5 (n = 8) followed by C6 (n = 7), C2 (n = 6, odontoid fractures), C7 (n = 4), C4 (n = 4) and one case of C3 and C1.
There were two false-positive cases in ultrasound where the vertebral body longitudinal length was reduced but CT showed no evidence of fracture.
Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of POCUS vs CT scan for vertebral body fracture were 40.9%, 96.8%, 81.8%, and 82.2% respectively.
Injuries not visible by POCUS
Injuries of the posterior column, transverse process fractures, pedicle fractures, upper cervical spine injury were not visible by POCUS but were identified by CT.
CONCLUSIONS
The authors concluded that while the curvilinear probe with wider field of view and better penetration makes it suitable to survey the C-spine from the anterior approach, the high rate of missed injuries makes POCUS an ineffective diagnostic tool for cervical spine injury.
Therefore, with these limitations, POCUS is unlikely to change management or prevent progression to more advanced imaging modalities.
 English
English
 Español
Español