ORIGINAL INVESTIGATION • Left Atrial Expansion Index for Noninvasive Estimation of Pulmonary Capillary Wedge Pressure: A Cardiac Catheterization Validation Study
Source: J Am Soc Echocardiogr 2021;34:1242-52
INTRODUCTION
Pulmonary capillary wedge pressure (PCWP) is pivotal in diagnosing and managing cardiac diseases. High PCWP, which is defined as PCWP > 12 mm Hg, can result from left ventricular (LV) diastolic dysfunction (DD). Right heart catheterization (RHC), an invasive and potentially risky procedure, is the gold standard technique for accurate hemodynamic assessment and PCWP measurement. However, it is reserved to only highly selected cardiac subgroups of patients.
In contrast, transthoracic echocardiography (TTE) is inexpensive, safe, available at the bedside, and easily repeatable. Therefore, it would be the ideal tool for noninvasive assessment of LV filling pressure (LVFP). The 2016 diastolic dysfunction guidelines provide a multiparametric algorithm for noninvasive LVFP and DD evaluation. However, the accuracy of the algorithm ranges from ranged from suboptimal to excellent.
Left atrial expansion index (LAEI) describes the relative left atrial (LA) volume changes during the reservoir phase of LA function. Because LA volume and its changes are related to LA pressure by LA volume-pressure curves, LAEI might be used as a noninvasive parameter for filling pressure (FP) evaluation.
The goals of this study were to:
1. Explore the correlation between LAEI and PCWP
2. Evaluate the independent and added value of LAEI for PCWP prediction over clinical and DD parameter
3. Compare the accuracy of LAEI for high PCWP identification head-to-head with the results of the 2016 DD algorithm
4. Derive and validate a simple equation for predicting PCWP from LAEI
METHODS
Study Population
This was a retrospective single-center study. 742 patients underwent both RHC and complete TTE within 24 hours. All patients were elective hospitalizations and did not have any changes in clinical status or medications between the two examinations.
Patients were excluded if they had inadequate TTE images or LA dedicated views, had mitral valve prostheses, surgical or transcatheter mitral valve repair or mitral stenosis. The final study population included 649 patients, randomly divided into derivation (n = 509) and validation (n = 140) cohorts.
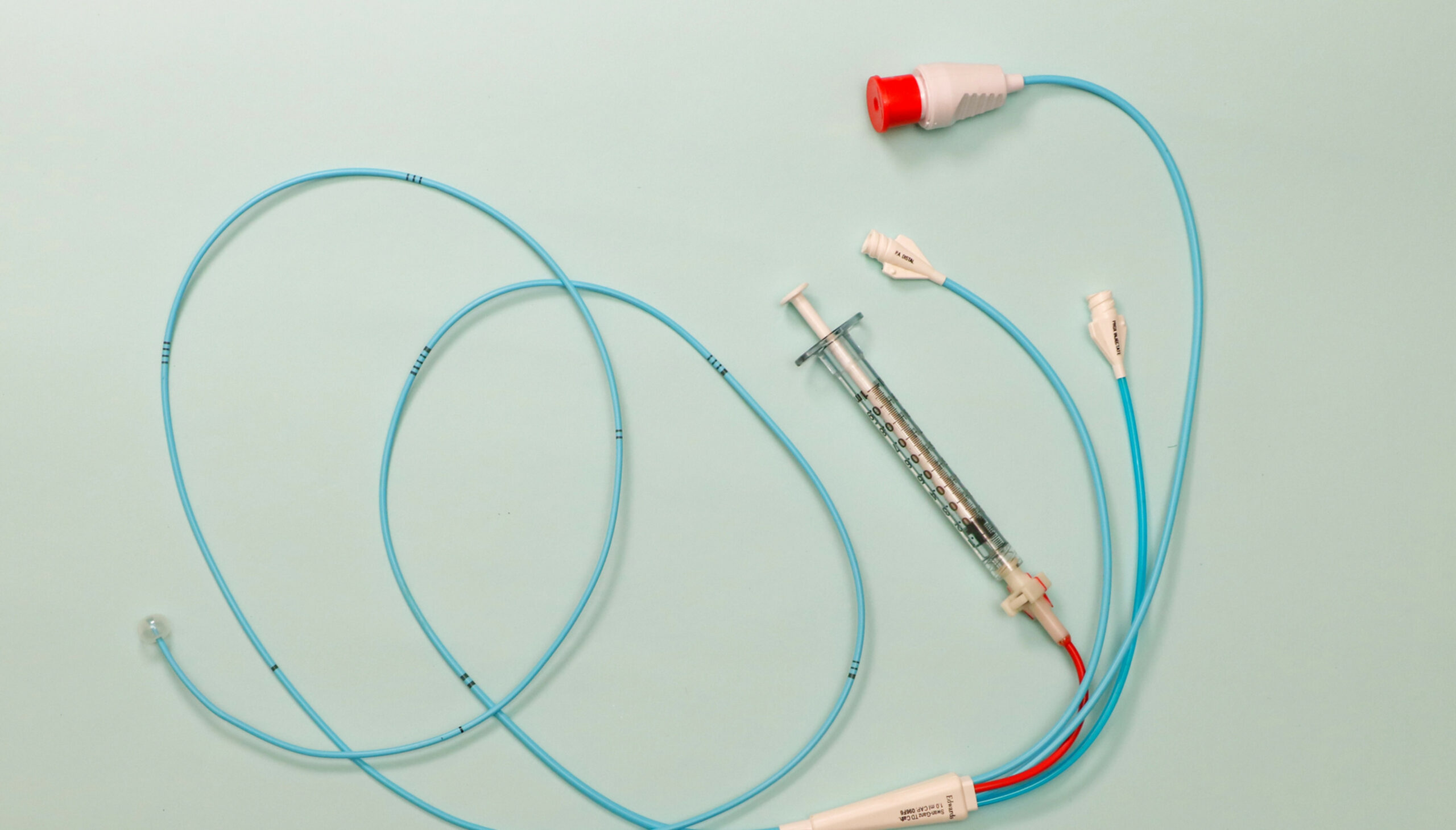
Right Heart Catheterization
RHC was performed with a Swan-Ganz catheter, following standard methodology, through a femoral transvenous approach. The Swan-Ganz catheter balloon was inflated and advanced until it reached the pulmonary capillary wedge position. The wedge position was identified by fluoroscopy, pressure waveform, and confirmed by pulmonary vein oxygen saturation (>95%) by a blood sample analysis drawn from the catheter tip.
Transthoracic Echocardiography
Transthoracic echocardiograms were exported, and standard measurements were performed offline according to American Society of Echocardiography and European Association of Cardiovascular Imaging guidelines by a reader blinded to clinical and RHC data, using a vendor-independent software package. TTE was performed before RHC in 88% of enrolled patients. Measurements included peak early (E) and late (A) mitral inflow velocities, E/A ratio, mitral annular septal and lateral early peak diastolic velocities (septal e’, lateral e’), E/e’ ratio, TRmaxVel, LV ejection fraction (LVEF) and mitral regurgitation (MR) severity. The 2016 DD algorithm was applied following the recommended stepwise evaluation of E/A ratio with E velocity, E/e’ ratio, TRmaxVel, and LAmaxVol, for both reduced and preserved LVEF.
LAEI was calculated as LAEI = [(LAmaxVol – LAminVol)/ LAminVol] x 100.
LAmaxVol was obtained with the biplane disk summation method from LA area tracings at end-systole in LA dedicated four- and two-chamber views. LAminVol was calculated similarly, with LA area tracings obtained at end-diastole. LA appendage and pulmonary veins were not included in LA tracings.
lnLAEI was derived by log transformation of LAEI.
RESULTS
Derivation Cohort Analysis
The derivation cohort was divided into subgroups with PCWP > 12 mm Hg (n = 251) and PCWP # 12 mm Hg (n = 258). Higher PCWP was associated with male gender, AF, faster HR, and higher body mass index.
PCWP > 12 mm Hg was associated with lower LAEI, larger left atrium, reduced LVEF, higher E/A ratio, higher E/e 0ratio, higher TRmaxVel, and more severe MR.
The diagnostic accuracy of lnLAEI for PCWP > 12 mm Hg identification was significantly higher than that of each DD parameter, with an optimal lnLAEI cutoff of <4.02.
Validation Cohort Analysis
Performance of the lnLAEI cutoff of <4.02 for identification of PCWP > 12 mm Hg was tested in the validation cohort in two different subgroups. The first validation subgroup (n = 98) excluded patients with AF and/or significant MR and compared lnLAEI < 4.02 against the 2016 DD algorithm The diagnostic accuracy of lnLAEI was higher than that of the 2016 DD algorithm (lnLAEI: sensitivity, 85%; specificity, 89%; accuracy, 88%; 2016 DD algorithm: sensitivity, 72%; specificity, 75%; accuracy, 74%).
Moreover, Cohen’s k coefficient of agreement with RHC was significantly higher for lnLAEI than for the 2016 DD algorithm (lnLAEI < 4.02, k = 0.71 6 0.07; 2016 DD algorithm, k = 0.45 6 0.09; P < .001).
CONCLUSION
The authors concluded that in patients with various chronic cardiac diseases, lnLAEI performed better than diastolic dysfunction parameters and the 2016 diastolic dysfunction algorithm for PCWP estimation.
They commented that their findings support the potential use of lnLAEI as an echocardiographic parameter for noninvasive PCWP estimation.
The equation PCWP = 38.3 – 6.2 x lnLAEI might provide supportive data in the context of a comprehensive multiparametric approach for PCWP evaluation.
 English
English
 Español
Español