RESEARCH • Doppler Study of Portal Vein and Renal Venous Velocity Predict the Appropriate Fluid Response to Diuretic in ICU: A Prospective Observational Echocardiographic Evaluation.
Source: Critical Care (2022) 26:305
INTRODUCTION
There has been a growing interest in the diagnosis and treatment of fluid overload and venous congestion in recent years. Fluid overload implies peripheral edema but also could result in pulmonary edema and venous congestion, which can alter tissue perfusion. Several studies have shown an association between fluid overload and morbidity and mortality in intensive care unit (ICU).
Recently, several ultrasound indices of venous congestion have been studied in the context of heart failure and/or cardio-renal syndrome. Measurement of portal pulsatility index, renal venous impedance, and/or the construction of the VEXUS score (venous ultrasound congestion score) are associated with venous congestion, occurrence of acute renal failure, and clinical prognosis of patients. Of these parameters, the pulsatility portal index and the venous renal flow are two promising parameters that have been associated with venous congestion and fluid overload.
The pulsatility portal index has been demonstrated to increase with fluid expansion when patients were unable to increase their cardiac output (i.e., fluid unresponsive). In the same way, the portal pulsatility index increase with the increase in positive end-expiratory pressure and central venous pressure.
Apart from these observations, the pulsatility portal index may reflect venous congestion in relation to volemia. The primary objective was to evaluate the ability of the portal pulsatility index to detect appropriate response to diuretic-induced fluid depletion. The secondary objectives were to evaluate the value of the renal venous impedance index and the VEXUS score to detect appropriate response to diuretic-induced fluid depletion.
METHODS
Patients
This was a prospective, observational, single-center study in a cardiovascular medico-surgical ICU of a tertiary university medical center.
The authors consecutively included all patients with age > 18 years, presence of clinical signs of fluid overload, absence of fluid responsiveness assessed by an increase in stroke volume following passing leg raising; and for whom the clinician decided to introduce loop diuretic treatment for several days.
Exclusion criteria included prior diuretic treatment during the ICU stays, permanent atrial fibrillation, veno-venous hemofiltration or dialysis, and patients with unstable shock (variation of blood pressure > 10% despite hemodynamic treatment and/or need to increase hemodynamic support).
Echocardiographic measurements
Transthoracic echocardiography was performed by an experienced physician according to current guidelines.
The echocardiographic parameters were calculated as the average of five measurements (regardless of the respiratory cycle). Data were acquired and stored for later analysis. The images were reviewed offline by an experienced operator blinded to the study outcomes. The attending physician was unaware of the results of the ultrasound examination. The LVEF (left ventricular ejection fraction) was measured using Simpson’s biplane method. The diameter of the LVOT (left ventricular outflow tract) was measured in a parasternal long-axis view upon patient inclusion. The AVA (aortic valve area, in cm2) was calculated as π × LVOT2/4. The VTIAo (aortic velocity–time integral) was measured by PW (pulsed wave) Doppler and a five-chamber apical view. SV (Stroke volume, in mL) was calculated as VTIAo × AVA, and CO (cardiac output, in L. min 1) as SV × HR (heart rate). In patients with TR (tricuspid regurgitation), peak TR velocity was measured by CW (continuous wave) Doppler, and the right ventricle–right atrium pressure gradient was calculated. The right ventricular systolic function was assessed by measuring TAPSE (tricuspid annular plane systolic excursion) and RVFAC (right ventricular fractional area change). The hepatic venous flow was recorded from the subcostal window.
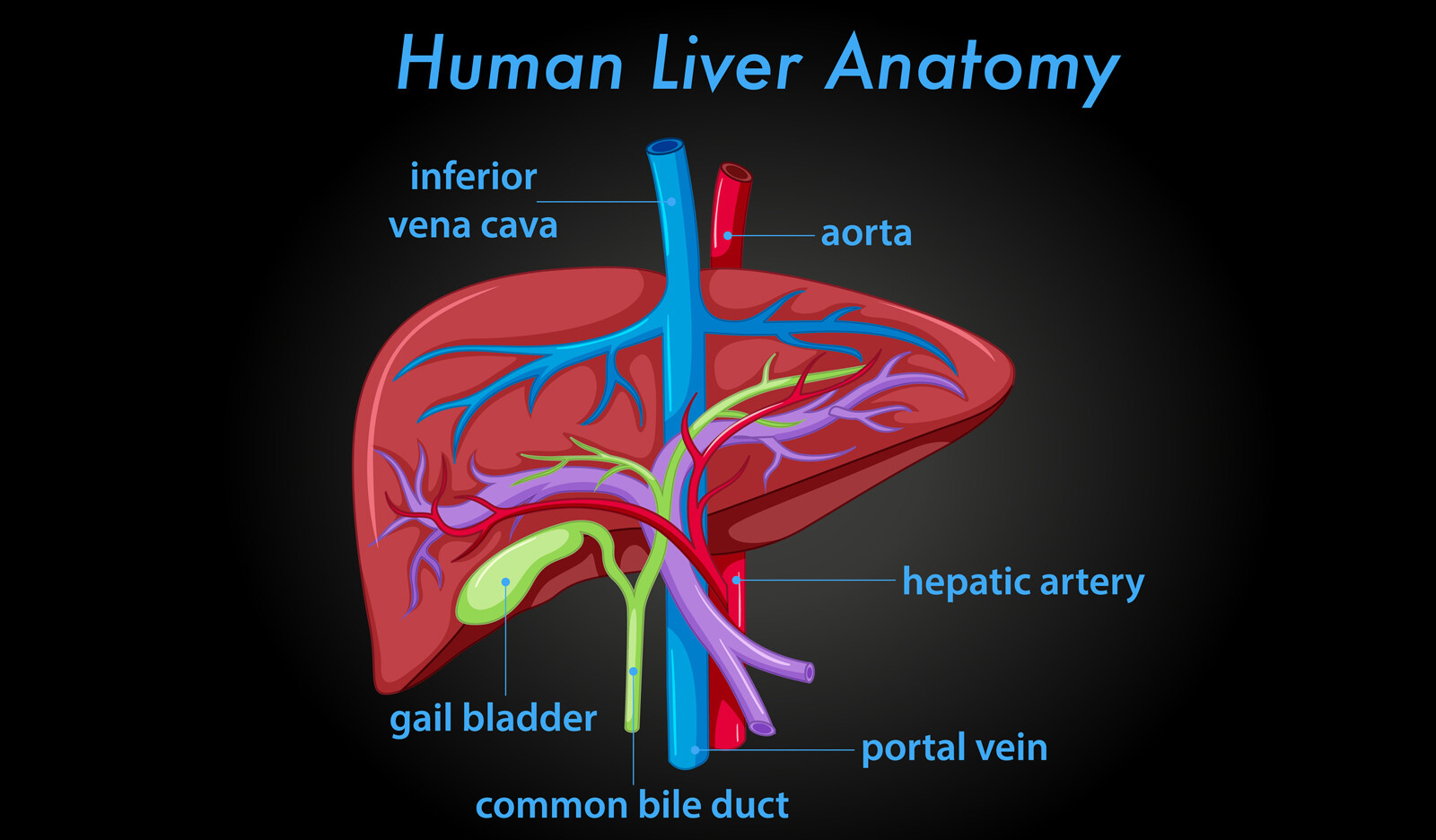
Portal, hepatic and renal Doppler measurements
The HV-S (supra-hepatic vein systolic) and HV-D (suprahepatic vein diastolic) velocities were measured, and the S/D (systolic/diastolic) ratio was calculated. With the patient in the supine position, the diameter of the inferior vena cava was measured in the subcostal view at 1 cm from its junction with the right atrium. The maximum and minimum diameters of the inferior vena cava were measured, and the percentage of change in diameter was calculated.
The PI (portal pulsatility index) was assessed by pulsed wave Doppler evaluation of the portal vein in the liver hilum.
Vmax (maximum velocity) and Vmin (minimum velocity) of the portal vein were measured in PW Doppler mode.
The portal PI was calculated using the following formula: PI = (Vmax − Vmin)/(Vmax).
RRI (Renal resistive index) and RVI (renal venous impedance index) were measured using a transparietal 5 MHz pulsed-wave Doppler probe.
RRI was calculated as:
RRI = (peak systolic velocity − end-diastolic velocity)/ peak systolic velocity. For each vein, RVI was calculated as: RVI = (peak systolic velocity − end-diastolic velocity)/peak systolic velocity. All values were the average of 3 measurements. RRI and RVI then were calculated as the average RRI and RVI for each kidney.
Definitions and scores
The authors constructed a congestion score based on clinical indicator and biomarkers of congestion:
- 0: No pulmonary rales/crackles
- 1: < 50% of lung
- 2: > 50% of lung
Peripheral edema:
- 0 – none
- 1 – ankle
- 2 – leg
- 3 – body
B-lines and/or lung ‘comets’:
- 0 – none
- 1 – more than 2 area
- 2– diffuse
Pleural effusion:
- 0 – none
- 1 – unilateral
- 2 – bilateral on lung ultrasound, and NT-proBNP (N-terminal pro B-type natriuretic peptide) value over 1500 pg mL−1
The congestion score ranged from 0 to 10, and a patient with a score ≥ 3 was considered as having significant clinical congestion.
Appropriate diuretic-induced fluid depletion was considered with a score lower than 3 at the end of the study for patients who had significant clinical congestion at baseline.
Patients with baseline congestion score lower than 3 or who did not lower the congestion score with diuretic were considered as the control group.
The percentage of fluid overload adjusted for body weight was calculated as ((total fluid in − total fluid out)/admission body weight × 100)
Study protocol
Patients were followed during all their ICU stay. The authors measured natriuresis and diuresis, as well as performed hemodynamic and echographic measurements two hours after diuretic treatment and compared the two.
Clinical examination, lung ultrasound, urine output, diuretic, vasoactive treatments, NT-proBNP, and blood creatinine were recorded at inclusion, 24 h later, and at ICU discharge. Cumulative fluid balance and cumulative percentage of fluid overload were calculated at inclusion, 24 h later, and at ICU discharge. The VEXUS score and the congestion score were calculated at inclusion and 2 h later.
The primary endpoint was the appropriate diuretic induced fluid depletion on the last day of ICU.
RESULTS
Population
Eighty-one patients with mean age of 68 ± 11 years (males: n = 51 (63%) and the median SAPS II of 46 ± 18 were included and analyzed in this study.
Diuretics were given for oliguria (n = 25), positive fluid balance (n = 63) and congestion (n = 18). Of the 81 patients, the median score was 3 (2–4), and 43 patients (53%) had a congestive score over 3.
The median change of congestion score between baseline and ICU discharge was − 1 (− 3–0).
Thirty-four patients (42%) have an appropriate response to diuretic-induced fluid depletion on the last day of ICU (i.e., a decrease in congestion score).
Comparison between patients with and without positive clinical response to diuretic‑induced fluid depletion
Two-hour diuresis and 2-hour natriuresis spots did not differ between the two groups: 558 ml (319) versus 683 ml (354), p = 0.137, and 91 mmol l−1 (33) versus 93 mmol l−1 (36), p = 0.87.
The VEXUS score was higher for patients with diuretic-induced fluid depletion than for the control group (2 (0–3) vs 0 (0–2), p = 0.03).
At baseline, the portal pulsatility index was higher in patients with appropriate diuretic-induced fluid depletion (45% (30–68) vs 28% (22–35), p = 0.001).
The venous impedance pattern was significantly worse in patients with appropriate diuretic-induced fluid depletion (2 (1–2) vs 3 (2–3), p = 0.011).
Assessment of the relationship between portal and renal flow parameters, VEXUS score, and the positive clinical response to diuretic‑induced fluid depletion
At baseline, the portal pulsatility index and venous impedance pattern were associated with the response to diuretic treatment.
When analyzed using multivariate logistic regression, portal pulsatility (OR = 20.9 (CI95% 2.8–158.9), p = 0.003), cardiac index (OR = 6.9 (CI 95 17–28.5), and the impedance venous pattern (OR = 6.3 (CI 95% 2.2–18.2) were associated with the diureticinduced fluid depletion response.
At 2 h, the portal pulsatility index and venous impedance pattern predicted with high specificity appropriate diuretic-induced fluid depletion.
CONCLUSION
The authors concluded that in this exploratory pragmatic study regarding the prediction of response to fluid depletion in ICU patients:
- patients with an appropriate response to diuretic-induced fluid depletion had high pulsatility portal index and worst renal venous impedance.
- Right- and left-sided echocardiographic parameters were not associated with an appropriate response to diuretic-induced fluid depletion.
- Pulsatility portal index and renal venous impedance were the best predictors of appropriate diuretic-induced fluid depletion response to diuretic.
- The changes in pulsatility portal index and venous renal index predicted the appropriate decongestion with fluid depletion but not response per se to diuretic therapy (amount of fluid).
- Pulsatility portal index and renal venous impedance are two parameters that may indicate that volume can be mobilized in a congestive state.
 English
English
 Español
Español