CASE REPORT • Perioperative Point-of-Care Ultrasound for Diagnosis of Acute Lower Extremity Arterial Thrombosis After Total Hip Arthroplasty Revision
Source: Can J Anesth 30 Dec 2021
The authors describe a 78-yr-old female patient with recurrent prosthetic join infections and dislocations who underwent right-sided stage II revision total hip arthroplasty. Her past medical history included decreased mobility due to chronic leg with associated non-ambulatory status for 18 months, essential thrombocytosis managed medically, and a cerebral vascular accident in 1990 with no residual deficits.
On the day of surgery, she was hemodynamically stable with preoperative palpable pulses documented in both lower extremities. An arterial line was placed as well as uncomplicated spinal anesthesia at L3/4. 17 mg of bupivacaine 0.5% (3.4 mL) with 15 lg of fentanyl were injected intrathecally. In the operating room, she underwent monitored anesthetic care (invasive and noninvasive blood pressure monitoring, 5-lead ECG, pulse oximetry, and capnography). A propofol infusion (50 •min-1) and a phenylephrine infusion (30 •min-1) were started, a one-time dose of 1.1 g of tranexamic acid was given at the start of surgery, and a single bolus of ketamine (10 mg) was given towards the end of surgery.
Surgery was complicated by a complex distal right femur fracture requiring significant extension of incision, and an open reduction and internal fixation. total operating room time was three hours 28 min.
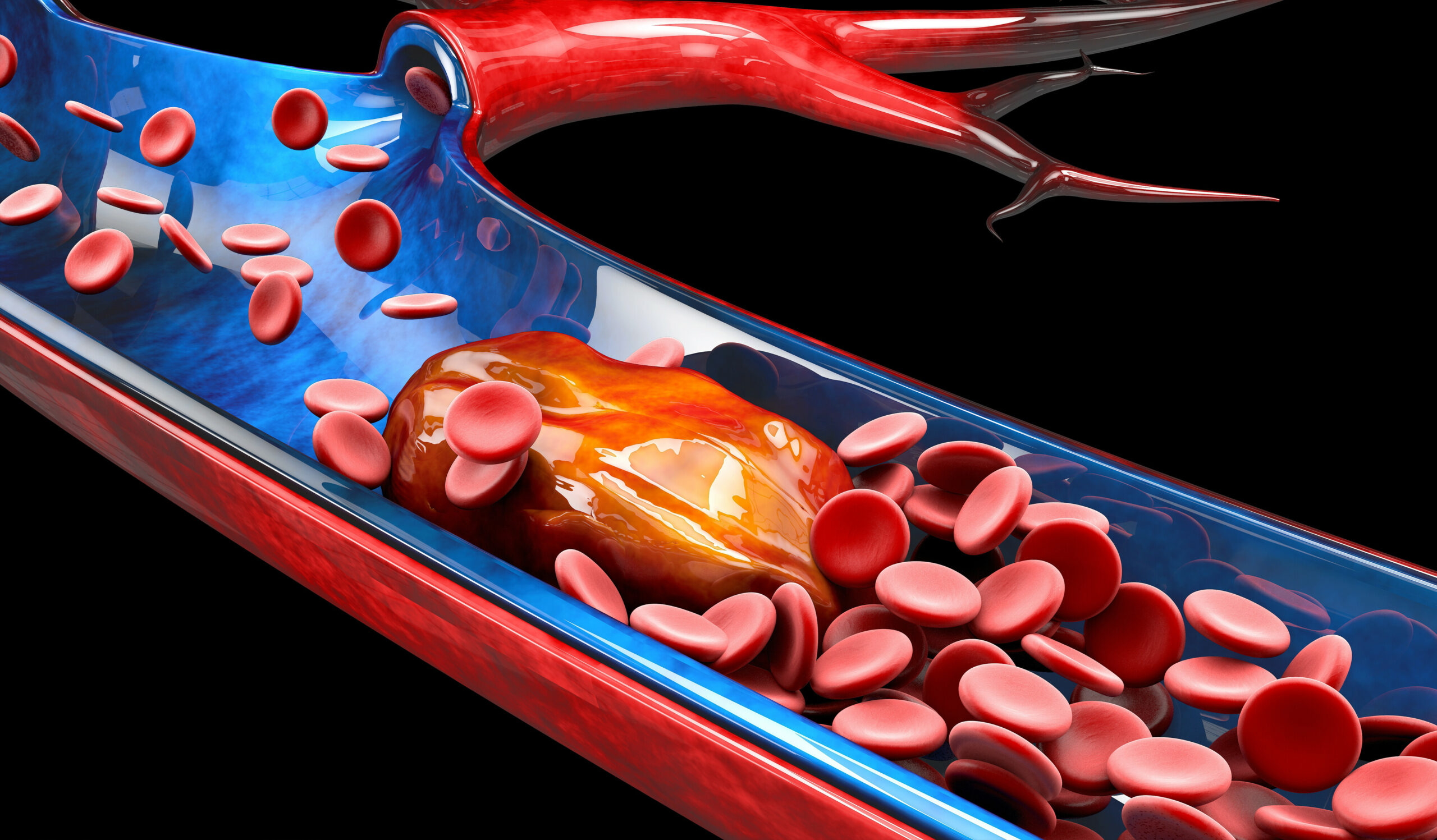
She was brought to the post anesthesia care unit (PACU) after successful completion surgery. In the PACU she had residual motor and sensory blockade, which was attributed to the spinal anesthesia. On initial routine assessment of perfusion in her operative leg, the PACU nurses were not able to identify a dorsalis pedis or a posterior tibial pulse on her operative leg with the audible-only Doppler. The anesthesia POCUS team, rounding on PACU patients for teaching purposes, offered assistance and used a vascular ultrasound probe to interrogate the dorsum of the patient’s right foot. The dorsalis pedis artery was identified by visual inspection but no flow was seen. Then, the distal posterior tibial artery was evaluated and demonstrated the absence of blood flow. The team then evaluated the popliteal artery, which was visually identified but no blood flow was appreciated. Finally, the common femoral artery was evaluated and flow was visualized at that level. When this artery was followed distally, cessation of arterial flow was seen in the superficial femoral artery. Hypoechoic lesion was observed in the superficial femoral artery.
While the patient appeared comfortable, she complained of moderate pain. There was some capillary refill and cool right extremity. Emergent vascular surgery referral was made for acute arterial occlusion of the superficial femoral artery. Evaluation by the vascular surgery team confirmed the findings and she underwent an emergent right common femoral artery thrombectomy with fasciotomy. The postoperative working diagnosis from the vascular surgical team was acute limb ischemia secondary to focal intimal injury of the proximal superficial femoral artery with in situ thrombosis. The discrepancy between the POCUS team finding of right superficial femoral artery occlusion and intraoperative thrombectomy of the right common femoral artery could be explained by the time difference between the POCUS evaluation and surgery, likely leading to clot extension into the common femoral artery.
The patient did very well, regained pulses in her leg and had returned to the referring hospital where she was working with physical and occupational therapists.
Discussion
In their conclusions, the author comment on the rare complication of acute arterial occlusion after hip arthroplasty, which can lead to devastating outcomes. In the immediate postoperative period, it may be difficult to rely on clinical presentation of acute limb ischemia to provide a timely diagnosis.
In the immediate postoperative period, many confounders, such as residual neuraxial anesthesia may prevent accurate assessment of pain, paresthesia, or paralysis in the PACU, and may interfere with the clinical diagnosis of acute limb ischemia. Other objective findings including capillary refill time are not reliable assessments of acute vascular disease. While vascular Doppler is routinely used for screen peripheral blood flow after orthopedic surgery, it has its limitations, such is inability to evaluate patients with foot ulcers or wounds and low sensitivity.
Therefore, the authors suggest considering POCUS evaluation initial screening of postoperative acute limb ischemia. They acknowledge that there is scarce information on the ultrasound appearance of acute peripheral arterial ischemia, but suggest that maybe extrapolating from carotid occlusions, the intraarterial thrombus may be either hyperechoic, hypoechoic, or mixed echoic depending on its composition. They propose that maybe in select patient populations, a POCUS arterial assessment may avoid the need for computed tomography angiography.
 English
English
 Español
Español