BRIEF RESEARCH COMMUNICATION • The Impact of Norepinephrine on Myocardial Perfusion in Critical Illness
Source: JASE 2021;34(9):1019-1020
BACKGROUND
In patients with cardiogenic shock, recent data suggest targeting higher mean arterial pressure (MAP) using norepinephrine reduces myocardial injury. However, impact of norepinephrine on coronary perfusion in critical illness has not been widely studied.
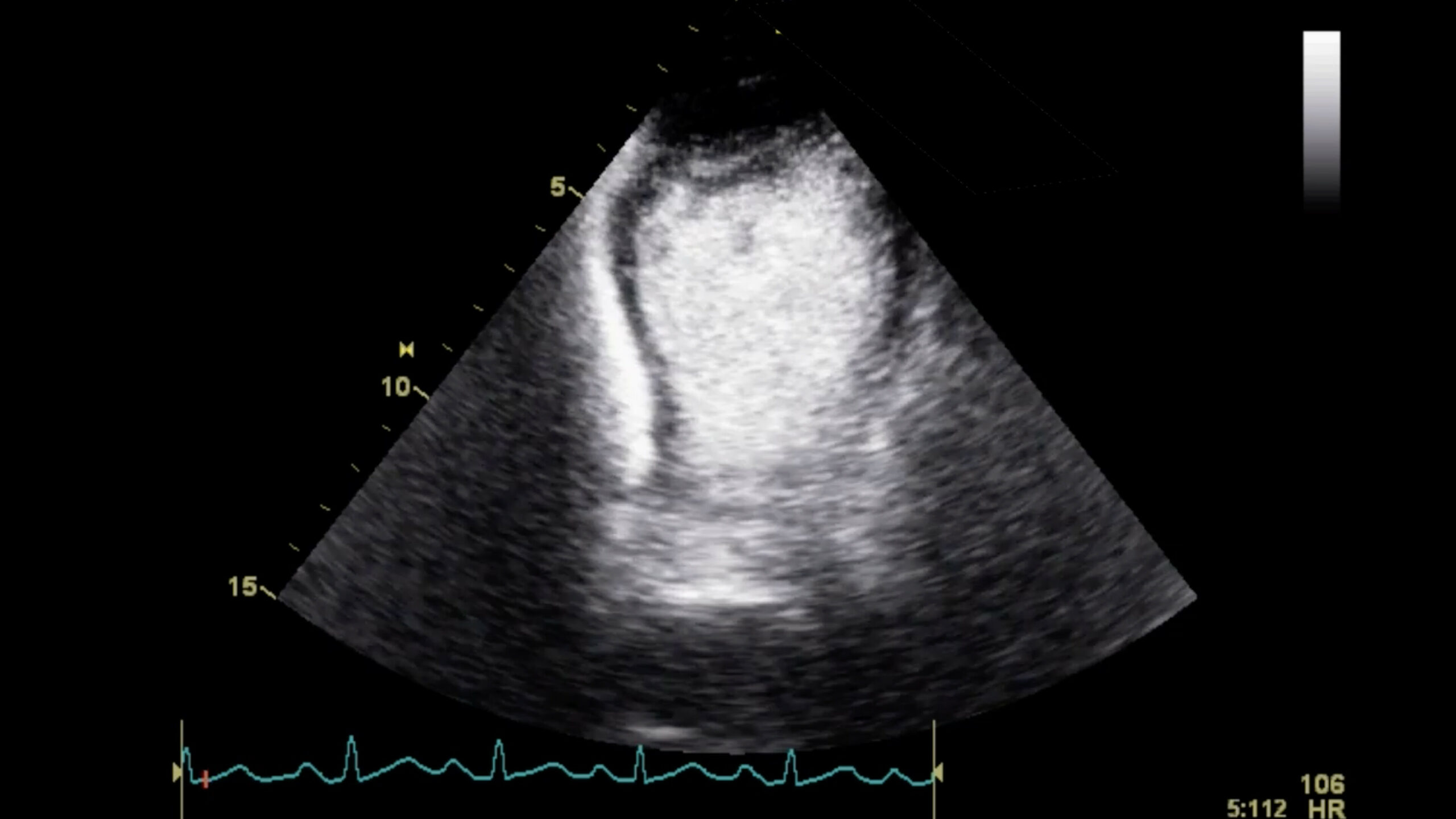
Myocardial contrast echocardiography (MCE) is a well-validated method of qualitative and quantitative assessment of myocardial perfusion in the noncritically ill. Therefore, the authors’ goal was to investigate whether MCE can be used to assess norepinephrine-related perfusion abnormalities that could be responsible for reduced left ventricular function.
METHODS
Twenty-two patients (18% female; age 46 6 15 years) were included in the study. Those patients with a history of coronary artery disease, regional wall motion abnormalities, or inadequate echocardiography images segments) were excluded.
The primary qualitative outcome measure was contrast intensity at 15 cycles post–destructive pulse using a previously validated semiquantitative scoring system. Quantitative assessment was performed to generate a surrogate of myocardial blood flow (MBF) using the accepted algorithm. Regions of interest were identified in the myocardium, taking care to avoid signals from the pericardium and left ventricular cavity.
RESULTS
At the time of MCE, patients’ hemodynamic parameters were:
- Heart rate: 90 beats per minute
- Systolic blood pressure: 94 mmHg
- Diastolic blood pressure: 69 mmHg
- Mean arterial pressure: 77 mmHg
Myocardial blood flow was negatively correlated with dose of norepinephrine (r = –0.69, P < .001), and was higher (P = .04) in patients on veno-venous extracorporeal membrane oxygenation.
Left ventricular ejection fraction did not correlate significantly with any measure of contrast perfusion such as MBF (r = 0.34, P = .12) or contrast intensity at 15 cycles post–destructive pulse (r = –0.1, P = .6) or with norepinephrine dose (r = –0.05, P = .8).
Contrast intensity at 15 cycles postdestructive pulse was negatively correlated with norepinephrine dose (r = –0.77, P < .001).
CONCLUSIONS
The authors concluded that in patients without coronary artery disease, norepinephrine may adversely impact myocardial perfusion in critical illness, independent of MAP.
They commented that the lack of association with MAP suggests that in critical illness, other factors predominate in determining coronary microvasculature function. They believe that in theory vasopressors may promote coronary perfusion by raising diastolic pressure, but they also raise systemic vascular resistance (afterload) and myocardial oxygen consumption (increased stroke work) which may explain these findings
 English
English
 Español
Español